Nurse practitioner, nurse anesthetist, nurse midwife, and clinical nurse specialist make up the advanced practice registered nurse class so frequently featured in U.S. News & World Report’s “best jobs.”
Although clinical nurse specialists (CNS) have an “excellent” job outlook, it’s the least talked-about option. So here are the facts about clinical nurse specialists.
What is a CNS? And what do they do?
Clinical nurse specialists (CNS) are clinical and health care leaders. They are advanced practice registered nurses (APRNs) who are certified in a niche nursing specialty where they have advanced knowledge and advanced clinical skills.
Clinical nurse specialists…
- Serve as educators, outcomes managers, consultants, researchers, change agents, and case managers, as well as clinical nurses
- Lead and collaborate in an interdisciplinary health care team that can include pharmacists, physical therapists, social workers, physicians, and advanced practice nurses
- Provide guidance and support to patients and their families in navigating the complex health care delivery system
Where do Clinical Nurse Specialists have practice authority?
Clinical Nurse Specialists have practice authority in many of the same states as nurse practitioners—and a few states that nurse practitioners don’t have practice authority in.
In these states, clinical nurse specialists and nurse practitioners have full practice authority.
In these states, clinical nurse specialists have practice authority but nurse practitioners do not.
What’s the difference between a CNS and a nurse practitioner?
Clinical nurse specialists manage the care of complex and vulnerable populations, educate and support interprofessional staff to provide optimal care through evidence-based best practices, and facilitate a culture of safety within health care systems.
Nurse practitioners practice autonomously and collaboratively with other health care providers to perform assessments, order laboratory and diagnostic tests, diagnose, prescribe medications and treatments, and perform procedures within their authorized scope of practice.
What are the educational requirements to become a CNS?
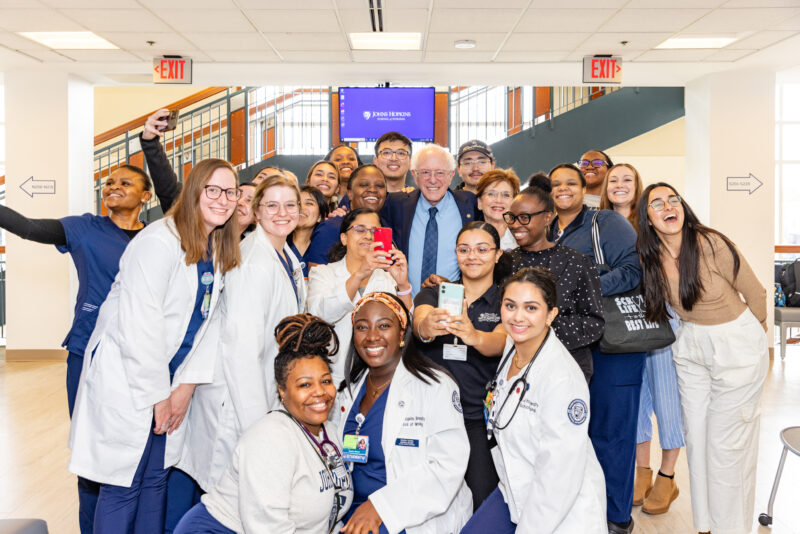
The Johns Hopkins School of Nursing offers three clinical nurse specialist tracks in the Doctor of Nursing Practice (DNP) Advanced Practice Track:
- Adult-Gerontological Health CNS
- Adult-Gerontological Critical Care CNS
- Pediatric Critical Care CNS
To be eligible for the program, you’ll need:
- A bachelor’s of science in nursing or entry-level master’s degree
- A current registered nurse (RN) license
- One year of full-time RN experience
Meet a CNS:
Bryan Hansen, PhD, RN, APRN-NS, ACNS-BC
 Assistant Professor & CNS Track Coordinator
Assistant Professor & CNS Track Coordinator
Bryan R. Hansen is a passionate advocate for the promotion of optimum mental health and well-being of older adults and their families through teaching, practice, and research.
Victoria Hughes, DNS, MSN, RN, CNS
Vickie Hughes has serviced in various clinical, educational, and leadership positions. She is an Adult Psychiatric/Mental Health CNS and a Certified Alcohol and Drug Abuse Counselor.
Laura Lucas, DNP, APRN-CNS, RNC-OB, C-EFM
 Assistant Professor & Clinical Coordinator, MSN (Entry into Nursing) Program
Assistant Professor & Clinical Coordinator, MSN (Entry into Nursing) Program
Laura Lucas most recently worked as a clinical nurse specialist at Johns Hopkins Hospital. She is certified in inpatient obstetrics, electronic fetal monitoring, and as an advanced practice CNS in Maryland.
Learn more:
- Doctor of Nursing Practice (DNP) Clinical Nurse Specialist
- Nurse Practitioner Vs. Clinical Nurse Specialist

ABOUT THE AUTHOR: SYDNEE LOGAN
Sydnee Logan is the Social Media and Digital Content Coordinator for Johns Hopkins School of Nursing. She shares what’s going on here with the world.